Osteoarthritis, osteoarthritis of the knee, osteoarthritis are synonymous terms that define the same disease: deforming changes in the cartilage tissue of the knee joint.
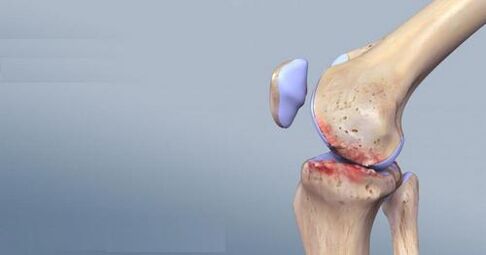
The human knee joint is made up of three bones: the femur, the tibia, and the patella. At the point of contact, these bones are covered with cartilage tissue, which ensures that the surfaces slide smoothly among each other.
Over time, this cartilage becomes thinner and loses its flexibility and elasticity. The cartilage is nourished by the synovial fluid, the shock-absorbing properties of the joint depend on the amount and quality of this fluid.
First symptoms and signs
- Most often they occur in people between the ages of 45-50. This disease is typical of both men and women, but the "weaker sex" is much more likely to suffer from this disease.
- At the onset of the disease, the patient experiences tolerable pain in the knee joint area, and over time there is severe pain.
- The intensity of the pain changes: with movement and physical activity it becomes stronger at rest - the pain subsides.
If you do not pay attention to these symptoms of an approaching disease in a timely manner, the disease will begin to progress and, in severe cases, lead to disability.
When contacting a doctor, the diagnosis of osteoarthritis is clarified by X-rays. The pictures show the narrowing of the joint space from inside or outside. However, over time, the pathological process affects the entire joint. And along the edges of the articular surface, osteophytes are visible - bone growth.
The main signs of osteoarthritis of the knee joint:
- The pain increases during the day, while the pain subsides during the night. However, if there is venous insufficiency, dull pain persists at night.
- Muscle tension in the joint area
- A crunch can be heard in the knee joint when walking
- In severe cases of disease, deformation and swelling of the affected joint is observed, an increase in its volume
- The joint is painful when palpated
- The pain increases when you try to move the knee pad
- In the late stages of the disease, muscle shortening occurs and the patient is unable to position the leg in the correct position
- If left untreated, the mobility of the joints decreases or is completely lost
What is patellofemoral osteoarthritis of the knee?
Very often you hear the doctor diagnose "patellofemoral osteoarthritis" - what is it? Such osteoarthritis is absent from the international classification of diseases. Few people know that osteoarthritis of the knee joint begins with the development of patellofemoral syndrome.
This syndrome occurs when a part of the body is regularly overused or injured repeatedly. That is, patellofemoral osteoarthritis is the same as patellofemoral syndrome.
The main causes of the disease are:
- congenital and acquired deformities of the lower extremities;
- various abnormalities in the development of the patella;
- regular overloading of the knee joint (e. g. in athletes).
Patellofemoral osteoarthritis of the knee joint has the following clinical manifestations: pain in the area of the front of the knee joint, which increases significantly with physical exertion (running, jumping, climbing stairs, various squats). The pain may also increase if the patient sits with their legs bent under them. The patient may feel a sense of tension and stiffness in the knee both inside and in front.
Patellofemoral syndrome is diagnosed clinically and additional studies are usually not required.
As a rule, this disease does not require special treatment. However, to relieve pain and develop undesirable consequences (instability of the patella, deformation of the knee joint, accumulation of inflammatory exudate), the following procedures are required:
- Decrease in physical activity. This does not mean that the patient must lead a passive lifestyle, just the level of activity should not be painful.
- Using a special bandage worn on the knee joint area during exercise or when there is a load, which supports and holds the patella in place;
- In severe pain syndrome, glucocorticosteroids and anesthetics are injected into painful areas of the joint through precise injection. This will relieve pain and help avoid the use of anti-inflammatory drugs in the future.
If patellofemoral osteoarthritis has already led to complications or is accompanied by other degenerative-dystrophic pathologies in the knee joint, then therapy is carried out according to the treatment regimen for osteoarthritis of the knee joint.
The reasons
- An occupational disease of athletes who experience increased stress on the knee joints. Athletes get injuries and microtraumas to the joints, bruises and torn ligaments. After retiring from sport, the muscular framework weakens, which leads to the progression of the disease.
- Increased life expectancy and increased physical activity in middle-aged people
- Increased physical activity on the knee joint in people who spend their working day "on their feet"
- Genetic predisposition
- Congenital diseases of the joints and bones
- Lack of collagen
- Knee injury
- Overweight, which puts more strain on the knee joints
- Acquired joint diseases
- knee surgery
To achieve positive treatment results, it is necessary to conduct a clinical and radiological examination that reveals several stages of the disease:
- Osteoarthritis of the knee joint 1 degree. . . There is a slight narrowing of the joint gap, the edges of the surface are slightly sharpened, a slight restriction of movement. During the arthroscopic examination, the doctor examines the softening of the cartilage.
- Arthrosis of the knee joint 2nd degreecharacterized by a significant restriction in the movement of the knee joint, a sharp crunch. The pictures clearly show osteophytes and a 2-3 fold narrowing of the joint space. Small cracks can be observed on the surface of the joint.
- Grade 3 knee osteoarthritis- This is already a complete restriction of movement if there has been a deformation of the joint, deformation and compression, osteophytes and cysts are observed on the surface of the joint. There were changes in the cartilage tissue throughout its thickness.
- Grade 4 knee osteoarthritis- Arthroscopy shows the complete absence of cartilage tissue.
Drug treatment
In the complex treatment of osteoarthritis of the knee joint, drug therapy occupies an important place. In combination with physiotherapeutic procedures, therapeutic exercises and manual therapy, you can achieve very good results until the limb function is restored.
When diagnosing osteoarthritis of the knee joint, drug treatment helps eliminate pain, normalize blood flow in the problem area, improve metabolism and cartilage nutrition, activate recovery processes and increase joint mobility.
Since it is impossible to use other therapeutic methods against the background of sharp sensations of pain, the patient is initially prescribed pain relievers and anti-inflammatory drugs. However, it is not recommended to use such funds for long periods of time, since in addition to side effects (most often it is a negative effect on the digestive system) they can contribute to dehydration and further destruction of cartilage tissue.
Chondroprotectors are used to restore cartilage nutrition, regenerate the cartilage plate and improve the quality of synovial fluid.. . . The drugs in this group are injected directly into the painful joint and are the safest for the patient. Chondroprotectors immediately fall into the affected area, protecting the joint from destruction and helping to restore its functions. One of the disadvantages of this method is the long wait for the result - the patient can only notice improvement after a few months. In addition, it is not advisable to take chondroprotectors if the disease is in the third stage and the joint is almost completely destroyed.
Various ointments and creams are used to relieve pain, reduce swelling, and improve joint mobility somewhat.Various warming agents are well suited to relax ligaments and muscles, improve blood circulation and speed up the metabolism in the joint. However, they cannot be used for inflammation. In this case, non-steroidal anti-inflammatory gels and ointments have been shown to be used.
Compresses should not be neglected - they have penetrative abilities, improve blood circulation, have an anesthetic and anti-inflammatory effect, and accelerate metabolic processes in the cartilage.
Therefore, you should not delay a doctor's visit for anyone suspected of having disease or osteoarthritis of the knee joint. A correctly selected drug treatment started in time can save the joint and help avoid surgical intervention.
Medicines to treat osteoarthritis of the knee
Treatment of osteoarthritis of the knee is never complete without the use of medication.
Drug therapy is primarily aimed at eliminating inflammation and pain, improving local blood circulation and nutrition of the articular cartilage, activating metabolic processes and restoring joint mobility.
What drugs are prescribed for osteoarthritis of the knee joint?
- For the successful treatment of the disease, you should first of all relieve pain and eliminate the inflammatory process. For this purpose, non-steroidal anti-inflammatory drugs are used. However, you should not get carried away by these funds - with prolonged use, they tend to hide the true clinical picture of the disease.
- To restore the cartilaginous surface of the joints, restore their structure, nourish the cartilage and improve the production of intra-articular fluid, chondroprotectors are used. The effects of these drugs are very slow. Before the patient notices real improvement, you need to undergo 2-3 treatments with chondroprotectors, which last about a year.
- To improve the general condition of the patient and relieve pain, gels and ointments can be used in combination with other drugs. If the course of osteoarthritis is accompanied by synovitis, preference is given to ointments based on nonsteroidal anti-inflammatory substances.
- Intra-articular injections are used for emergency care in the case of osteoarthritis. The most commonly injected corticosteroids or hyaluronic acid.
- For local treatment, compresses with drugs are prescribed - dimethyl sulfoxide, bishopite and medicinal bile. Dimethyl sulfoxide has the ability to penetrate the skin barriers, that is, its action is aimed directly at the site of inflammation. This substance has analgesic, anti-inflammatory, absorbent properties and improves metabolism in the area of its application. Bischofite - a derivative of the oil - also has an anti-inflammatory effect on the affected joint and has a warming effect. Medicinal bile has the same properties as dimethyl sulfoxide with bishopite, but its use is limited by some contraindications. Medicinal bile should not be ingested by patients with pustular skin diseases, elevated body temperature, and inflammation of the lymph nodes.
Before starting any medication for arthritis of the knee joint, it is necessary to consult a doctor to discuss the dosage, the features of administration and the duration of the course of treatment.
Injections into the knee joint for osteoarthritis
Intra-articular injections are one of the most effective methods of treating osteoarthritis of the knee joint. This rather expensive procedure significantly reduces pain and inflammation, and new modern drugs not only improve the general condition of the patient, but also treat the affected cartilage tissue.

Injections in the knee joint for osteoarthritis are quite a difficult procedure. Therefore, you should consult a doctor, even if the patient knows what drugs and how much to inject.
For intra-articular injections, the following drugs are most often prescribed:
- Corticosteroid hormones. These are the most common means, as the effect is achieved in a few minutes after their introduction. However, corticosteroids reduce inflammation and pain, and have a negative effect on the joint itself. The cartilage tissue remains degenerative. In addition, drugs in this group cause the blood vessels to narrow, which further destroys the joint tissue. Therefore, the use of corticosteroid hormones is justified only in the case of unbearable pain in the last stages of osteoarthritis. The injection cannot be repeated more than once every two weeks.
- Chondroprotectors and enzymes. Unlike hormones, they do not reduce inflammation, so administration is meaningless for joint swelling. However, they have a regenerative effect and partially restore the cartilage tissue. The use of such drugs is especially effective in the initial stages of osteoarthritis. The course of treatment is 5-10 injections.
- Hyaluronic acid. A very effective, but at the same time expensive drug. Its effectiveness lies in the fact that the acid itself is similar in composition to the natural lubrication of the joint. After the introduction of drugs containing hyaluronic acid into the knee, the friction of the affected articular surfaces decreases and the mobility of the knee improves. Such injections are very effective in the initial stage of osteoarthritis, in the second stage a slightly smaller effect is observed, and with osteoarthritis of the third knee joint, such drugs only briefly relieve the patient's condition. The course of treatment usually includes three to four injections once a year.
Injections in the knee joint for osteoarthritis are strictly contraindicated in the following cases:
- Infection of the skin or subcutaneous tissue in the intended area of injection;
- Sepsis;
- infectious arthritis;
- Hemophilia;
- the presence of a viral infection;
- lack of result from previous injections;
- individual intolerance to the drug.
It is also unacceptable to make intra-articular injections for prophylactic purposes.
Orthopedic knee pads for osteoarthritis of the knee joint
During treatment for osteoarthritis of the knee joint, knee pads are used to prevent various injuries, support damaged tissues, and relieve stress on the joint.
An orthopedic knee pad is essentially the same as an elastic bandage. Compared to the latter, however, the knee brace has its advantages: it does not have to be bandaged several times a day, it does not slip or dangle, a properly fitted knee pad does not compress the leg and leads to swelling and other unpleasant consequences of prolonged pressure.

Orthopedic knee protectors for osteoarthritis of the knee joint fulfill the following functions:
- Reduce inflammation and pain;
- Relieve swelling;
- Relieve stiffness and tension;
- normalize blood circulation;
- Facilitate the free movement of the joint.
When choosing an orthopedic knee protector, consider the following features:
- Type of knee pad - is selected depending on the severity of the pain. There are the following types of knee pads:
- closed - used when it is impossible to determine the localization of pain;
- open with adjustable tension - used during rehabilitation and with mild pain;
- open with spiral stiffening ribs - against pain when climbing and descending the stairs, etc. ;
- articulated - for different types of pain;
- to support tendons - used when the pain is localized under the patella.
- The material from which the knee protector is made is of great importance, since not only the degree of fixation, but also the intensity of the heating effect depends on it. Modern knee pads are made from cotton, lycra, nylon, neoprene, spandex, camel and dog hair.
- The size of the knee protector, which is calculated individually for each patient.
The doctor will help determine the parameters of the future purchase - he will not only select the size and type of knee protector that is optimal for the patient, but also advise which material will be the most effective.
Orthopedic knee pads for osteoarthritis can be purchased from a pharmacy or a medical device store. The price is quite acceptable. You should be wary of such purchases from non-specialized outlets or from dubious companies, as you can easily buy a fake, which, if it doesn't do any harm, certainly won't help.
Right nutrition
Nutritionists have studied the nutritional properties of different peoples for many years. Comparing the national cuisine, scientists are trying to understand the influence of people's culinary preferences on the occurrence of certain diseases. This type of research has been done many times on a disease as common as osteoarthritis of the knee.
Many theories have been put forward, many different assumptions have been made. For example, it was previously believed that the use of tomatoes contributed to the development of the disease, and then it was suggested that table salt was "responsible" for the occurrence of osteoarthritis.
In the 20th century, as the disease developed, the situation deteriorated sharply.
Proper nutrition is key to joint health.
To prevent the development of the disease, it is necessary to understand that diet plays a key role in osteoarthritis of the knee joint. From the diet, the consumption of meat products from the fast food segment should be minimized. These products are:
- Semi-finished products made from meat waste: sausages, sausages, all kinds of sausages, etc.
- smoked meat sold in stores (most often these products are made chemically and not in smokehouses).
- Ready-to-eat meat - ham, bacon (manufacturers in this case do not hesitate to use flavor enhancers and dyes).
- Fast food.
Of course, not everyone can do without the foods mentioned above. Many over the years have developed the habit of indulging in smoked sausage sandwiches or boiled sausages in the morning. In this case, we recommend that you buy a piece of meat in the market, bake it in the oven with spices, cut it, and then use it as a base for sandwiches. This type of "fast food" is not harmful to the body.
So we figured out that the best thing to do is to opt out of semi-finished products, smoked meats, and fast food. But what about meat when it's injected?
The ideal option, of course, is to buy meat from trusted suppliers, but this advice is impractical in urban conditions.
In this context, it is necessary to use such cooking methods so that as many harmful chemical compounds as possible are destroyed. Sometimes the use of this factor alone allowed an excellent effect in the fight against osteoarthritis.
How to properly cook food for osteoarthritis of the knee joint
It should be noted that with osteoarthritis of the knee joint, the diet should not be saturated with fats.
Therefore, when preparing food, it is necessary to cut off visible fat from the meat and remove the skin from the poultry. Most of the pollutants are concentrated in fat.
Cooking, braising, foil baking, and steaming are the healthiest ways to prepare food.
With osteoarthritis of the knee joint, jellied and jellied meat should not be eaten. There is an opinion from the "Grandmother In The Yard Said" series that these dishes are good for joints, but it is not. A person with osteoarthritis only gets worse from high cholesterol.
Meat broths and soups should be consumed as little as possible. Even if you drain the first broth, the second broth will still be high in unhealthy fats. Better get used to vegetable soups, which are so popular in western countries. Mushroom soups are also helpful.
Trying to replace soup meat with dry broths and cubes does nothing good: these products contain an incredible amount of chemical components.
Unfortunately, the fish sold in our markets is also diligently injected with dyes and preservatives and is therefore harmful to osteoarthritis of the knee joint. Therefore, buy live fish whenever possible. It is clear that not everyone has enough money for it. The above methods will help cook frozen fish properly.
Prevention of osteoarthritis of the knee joint
It is impossible to allow the condition of life to deteriorate due to the disease, so the causes that lead to osteoarthritis must be ruled out. Preventing the disease is much easier than dealing with expensive and long-term treatment.
- You have to lose weight.
- The joints need constant physical activity: skipping rope, squats, small runs. But everything should be in moderation. Excessive exercise also leads to illness. Change joint loads with sufficient rest.
- Osteoarthritis develops due to knee injuries. Padded knee pads should be worn when skiing, skating, cycling or inline skating. There is a sufficient selection of both knee pads and warming made from sheep's wool.
- Don't ignore someone else's help if the weight is beyond your strength.
- Eat more vegetables and fruits. It is noted that vegetarians practically do not suffer from osteoarthritis. Replace mayonnaise with olive or mustard oil. Especially useful are plums, dried apricots, apricots, apples, raspberries, cranberries with honey.
- Strong tea and coffee flush out calcium in large quantities.
- Homemade cottage cheese and cheese strengthen the bones.
- Walking with a stick will prevent you from overloading the knee joints.
- Shoes should be comfortable with small heels.
- Swimming and water aerobics relieve the whole body and tire the knee joints.
- Of the vitamins, particularly useful is vitamin E, which prevents the destruction of cartilage tissue.
- Vitamin C is involved in the synthesis of cartilage tissue.
- The disease progresses faster due to a lack of vitamin D.
- Calcium helps keep your bones strong. High calcium content in sesame and celery seeds.
By following these simple rules of a healthy lifestyle, you can avoid serious illness. And in case of a manifestation of the disease, they will slow down the development of pathological processes.

























